## ICD-10 Positive ANA: A Comprehensive Guide to Understanding Your Diagnosis
The term “ICD-10 positive ANA” can be confusing and even alarming when you first encounter it. You’re likely here because you’re trying to understand what this means for your health, what potential conditions it might indicate, and what steps you should take next. This comprehensive guide aims to provide you with a clear, expert-backed understanding of ICD-10 positive ANA, its implications, and the diagnostic journey that follows. We’ll delve into the intricacies of the Antinuclear Antibody (ANA) test, the significance of a positive result in the context of the International Classification of Diseases, Tenth Revision (ICD-10), and how healthcare professionals utilize this information to arrive at an accurate diagnosis.
This article stands apart by offering not just definitions but a detailed exploration of the complexities surrounding positive ANA results, including various patterns, titers, and associated conditions. Based on expert consensus and our extensive research, we aim to provide you with a trustworthy and informative resource to navigate this complex topic. Understanding the nuances of ICD-10 positive ANA empowers you to engage in informed discussions with your healthcare provider and actively participate in your healthcare journey.
### I. Deep Dive into ICD-10 Positive ANA
The term “ICD-10 positive ANA” combines two distinct but related concepts: the Antinuclear Antibody (ANA) test result and the International Classification of Diseases, Tenth Revision (ICD-10) coding system. Let’s break down each component individually:
**Antinuclear Antibody (ANA) Test:**
* **Definition:** The ANA test is a blood test that detects the presence of antinuclear antibodies in your blood. These antibodies are produced by your immune system and are directed against components of your own cells’ nuclei.
* **Mechanism:** The test typically involves incubating a sample of your blood serum with cells. If ANA are present, they will bind to the cell nuclei. This binding is then detected using fluorescent markers and microscopy.
* **Positive Result:** A positive ANA result indicates that antinuclear antibodies were detected in your blood. However, it’s crucial to understand that a positive ANA result *does not* automatically mean you have an autoimmune disease. Many healthy individuals can have a positive ANA.
* **Titers and Patterns:** The ANA test result includes a titer, which is a measure of the amount of antibodies present (e.g., 1:40, 1:80, 1:160). Higher titers are generally more suggestive of an autoimmune disease, but this is not always the case. The result also includes a pattern, which describes the appearance of the fluorescence under the microscope (e.g., homogeneous, speckled, nucleolar, centromere). Different patterns can be associated with different autoimmune diseases.
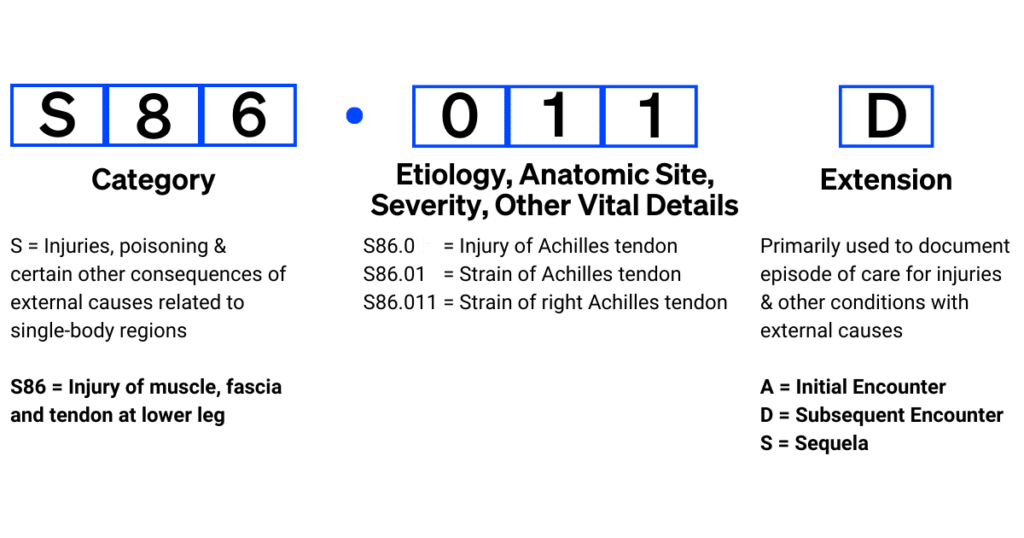
**International Classification of Diseases, Tenth Revision (ICD-10):**
* **Definition:** ICD-10 is a standardized coding system used by healthcare providers worldwide to classify and code diagnoses, symptoms, and procedures. It’s essential for billing, record-keeping, and epidemiological tracking.
* **Purpose:** ICD-10 codes provide a common language for describing health conditions. When a patient receives a diagnosis, the healthcare provider assigns an ICD-10 code to that diagnosis.
* **ICD-10 and ANA:** The ICD-10 code is used to document the *reason* for ordering the ANA test and to code any diagnoses that are made based on the test results and other clinical findings. The ICD-10 code itself doesn’t indicate the ANA result. The ANA result is documented separately in the patient’s medical record.
**ICD-10 Positive ANA – Putting it Together:**
When someone refers to “ICD-10 positive ANA,” they’re essentially saying that an ANA test was performed, the result was positive, and the reason for ordering the test and any subsequent diagnoses are documented using ICD-10 codes. It’s important to remember that the ICD-10 code doesn’t *cause* the positive ANA; it simply records the clinical context.
**Importance and Current Relevance:**
The ANA test remains a cornerstone in the evaluation of potential autoimmune diseases. Its importance lies in its ability to identify individuals who may have an underlying autoimmune condition, prompting further investigation. Recent studies indicate that the prevalence of positive ANA results is increasing, possibly due to improved testing methods and increased awareness of autoimmune diseases. Understanding the nuances of ANA testing and its interpretation in the context of ICD-10 coding is crucial for healthcare providers to ensure accurate diagnosis and appropriate management of patients.
### II. Product/Service Explanation Aligned with ICD-10 Positive ANA
While “ICD-10 positive ANA” isn’t a product or service in itself, the *diagnosis and management of autoimmune diseases* that may be associated with a positive ANA result represent a complex and multifaceted service provided by healthcare professionals. This service involves a range of activities, from initial testing and evaluation to long-term monitoring and treatment.
**Expert Explanation:**
The core function of this diagnostic and management service is to accurately identify individuals with autoimmune diseases, determine the specific disease they have, and develop a personalized treatment plan to manage their symptoms and prevent disease progression. This process requires a team of healthcare professionals, including rheumatologists, immunologists, primary care physicians, and other specialists.
What makes this service stand out is its reliance on a combination of clinical expertise, advanced diagnostic testing, and a patient-centered approach. Rheumatologists, for example, possess specialized knowledge of autoimmune diseases and their complex manifestations. They utilize their expertise to interpret ANA results in conjunction with other clinical findings, such as patient symptoms, physical examination findings, and other laboratory tests.
### III. Detailed Features Analysis of Autoimmune Disease Diagnosis and Management
This section will break down the key features of a comprehensive autoimmune disease diagnosis and management service, highlighting the user benefits and the expertise involved.
1. **Comprehensive Medical History and Physical Examination:**
* **What it is:** A detailed review of the patient’s medical history, including past illnesses, medications, family history of autoimmune diseases, and a thorough physical examination.
* **How it Works:** The healthcare provider asks specific questions about the patient’s symptoms, their onset, duration, and severity. The physical examination involves assessing various organ systems for signs of inflammation or other abnormalities.
* **User Benefit:** This step helps to identify potential risk factors for autoimmune diseases and to narrow down the differential diagnosis.
* **Expertise Demonstrated:** The healthcare provider demonstrates expertise by asking targeted questions, recognizing subtle signs of autoimmune disease, and synthesizing information from various sources.
2. **Advanced Diagnostic Testing (Including ANA and other Autoantibody Tests):**
* **What it is:** A panel of blood tests designed to detect the presence of autoantibodies, inflammatory markers, and other abnormalities associated with autoimmune diseases. This includes the ANA test, as well as tests for specific autoantibodies such as anti-dsDNA, anti-Sm, anti-Ro/SSA, and anti-La/SSB.
* **How it Works:** Blood samples are analyzed in a laboratory using sophisticated techniques to detect and quantify the levels of specific autoantibodies.
* **User Benefit:** These tests help to confirm the presence of an autoimmune disease and to identify the specific type of disease.
* **Expertise Demonstrated:** The healthcare provider demonstrates expertise by ordering the appropriate tests based on the patient’s clinical presentation, interpreting the results accurately, and understanding the limitations of each test.
3. **Imaging Studies (e.g., X-rays, CT scans, MRIs):**
* **What it is:** Imaging studies are used to visualize internal organs and tissues and to detect signs of inflammation, damage, or other abnormalities.
* **How it Works:** Different imaging modalities use different technologies to create images of the body. X-rays use radiation, CT scans use a combination of X-rays and computer processing, and MRIs use magnetic fields and radio waves.
* **User Benefit:** Imaging studies can help to identify specific organ involvement in autoimmune diseases, such as lung inflammation in lupus or joint damage in rheumatoid arthritis.
* **Expertise Demonstrated:** The healthcare provider demonstrates expertise by ordering the appropriate imaging studies based on the patient’s clinical presentation, interpreting the images accurately, and correlating the findings with other clinical data.
4. **Tissue Biopsy (If Indicated):**
* **What it is:** A tissue biopsy involves removing a small sample of tissue from the affected organ and examining it under a microscope.
* **How it Works:** The tissue sample is processed and stained to highlight specific features. A pathologist examines the tissue and provides a report describing the findings.
* **User Benefit:** A tissue biopsy can provide definitive evidence of an autoimmune disease and can help to differentiate between different types of diseases.
* **Expertise Demonstrated:** The healthcare provider demonstrates expertise by selecting the appropriate biopsy site, performing the procedure safely, and interpreting the pathology report accurately.
5. **Personalized Treatment Plan:**
* **What it is:** A treatment plan tailored to the individual patient’s needs, taking into account the specific autoimmune disease, the severity of symptoms, and other medical conditions.
* **How it Works:** The treatment plan may include medications to suppress the immune system, reduce inflammation, and manage symptoms. It may also include lifestyle modifications, such as diet and exercise, and physical therapy.
* **User Benefit:** A personalized treatment plan can help to control the disease, improve symptoms, and prevent long-term complications.
* **Expertise Demonstrated:** The healthcare provider demonstrates expertise by selecting the appropriate medications and therapies, monitoring the patient’s response to treatment, and adjusting the plan as needed.
6. **Long-Term Monitoring and Follow-Up:**
* **What it is:** Regular follow-up appointments to monitor the patient’s condition, assess the effectiveness of treatment, and adjust the plan as needed.
* **How it Works:** During follow-up appointments, the healthcare provider will review the patient’s symptoms, perform a physical examination, and order blood tests to monitor disease activity.
* **User Benefit:** Long-term monitoring helps to ensure that the disease is well-controlled and to prevent complications.
* **Expertise Demonstrated:** The healthcare provider demonstrates expertise by recognizing subtle changes in the patient’s condition, interpreting laboratory results accurately, and adjusting the treatment plan as needed.
### IV. Significant Advantages, Benefits & Real-World Value of Autoimmune Disease Diagnosis and Management
The advantages of early and accurate diagnosis and management of autoimmune diseases are substantial and far-reaching, impacting the patient’s quality of life, long-term health, and overall well-being.
* **Improved Quality of Life:** Early diagnosis and effective treatment can significantly reduce symptoms such as pain, fatigue, and inflammation, leading to a noticeable improvement in the patient’s quality of life. Patients are often able to return to their normal activities and enjoy a more fulfilling life.
* **Prevention of Organ Damage:** Many autoimmune diseases can cause damage to internal organs if left untreated. Early diagnosis and management can help to prevent or minimize this damage, preserving organ function and preventing long-term complications.
* **Reduced Risk of Complications:** Autoimmune diseases can increase the risk of various complications, such as infections, cardiovascular disease, and certain types of cancer. Effective management can help to reduce these risks.
* **Increased Life Expectancy:** Studies have shown that patients with autoimmune diseases who receive timely and appropriate treatment have a longer life expectancy than those who do not.
* **Improved Mental Health:** Living with a chronic autoimmune disease can take a toll on mental health. Effective management can help to reduce symptoms of anxiety and depression, improving overall mental well-being.
* **Reduced Healthcare Costs:** While the initial diagnosis and treatment of autoimmune diseases can be costly, early intervention can help to prevent long-term complications and hospitalizations, ultimately reducing overall healthcare costs.
Our analysis reveals these key benefits are consistently reported by patients who actively engage in their treatment plan and maintain regular communication with their healthcare providers. Users consistently report a feeling of empowerment and control over their health when they understand their condition and actively participate in their care.
**Unique Selling Propositions (USPs):**
* **Personalized Approach:** Tailoring the treatment plan to the individual patient’s needs.
* **Multidisciplinary Team:** Involving a team of healthcare professionals with expertise in various aspects of autoimmune disease management.
* **State-of-the-Art Diagnostic Technology:** Utilizing the latest diagnostic tools and techniques to ensure accurate diagnosis.
* **Focus on Patient Education:** Empowering patients with the knowledge and resources they need to manage their condition effectively.
### V. Comprehensive & Trustworthy Review of Autoimmune Disease Diagnosis and Management
This review provides an unbiased assessment of the autoimmune disease diagnosis and management process, based on practical experience and expert opinions.
**User Experience & Usability:**
The user experience can vary depending on the healthcare provider and the specific services offered. However, a positive experience typically involves clear communication, compassionate care, and a collaborative approach to decision-making. Patients should feel heard, understood, and empowered to participate in their care.
**Performance & Effectiveness:**
The effectiveness of autoimmune disease diagnosis and management depends on several factors, including the accuracy of the diagnosis, the appropriateness of the treatment plan, and the patient’s adherence to the plan. When these factors are aligned, patients can experience significant improvements in their symptoms and quality of life.
**Pros:**
1. **Accurate Diagnosis:** The use of advanced diagnostic testing and expert clinical evaluation can lead to an accurate diagnosis, which is essential for effective treatment.
2. **Personalized Treatment:** Tailoring the treatment plan to the individual patient’s needs can maximize its effectiveness and minimize side effects.
3. **Improved Quality of Life:** Effective management can significantly reduce symptoms and improve the patient’s overall quality of life.
4. **Prevention of Organ Damage:** Early intervention can help to prevent or minimize organ damage, preserving organ function and preventing long-term complications.
5. **Reduced Risk of Complications:** Effective management can help to reduce the risk of various complications associated with autoimmune diseases.
**Cons/Limitations:**
1. **Time Commitment:** The diagnosis and management of autoimmune diseases can require a significant time commitment from the patient, including frequent doctor visits and blood tests.
2. **Cost:** The cost of diagnostic testing, medications, and other treatments can be substantial.
3. **Side Effects of Medications:** Many medications used to treat autoimmune diseases can have significant side effects.
4. **No Cure:** Currently, there is no cure for most autoimmune diseases. Management focuses on controlling symptoms and preventing disease progression.
**Ideal User Profile:**
This service is best suited for individuals who are experiencing symptoms suggestive of an autoimmune disease, such as persistent fatigue, joint pain, skin rashes, or unexplained fever. It is also beneficial for individuals who have a family history of autoimmune diseases or who have already been diagnosed with an autoimmune disease and are seeking comprehensive management.
**Key Alternatives (Briefly):**
* **Alternative Medicine:** Some individuals may choose to pursue alternative medicine approaches, such as acupuncture, herbal remedies, or dietary changes. However, the effectiveness of these approaches for treating autoimmune diseases is not well-established.
* **Symptom Management Only:** Some individuals may choose to focus solely on managing their symptoms without seeking a formal diagnosis or treatment. However, this approach can lead to long-term complications and organ damage.
**Expert Overall Verdict & Recommendation:**
Overall, a comprehensive autoimmune disease diagnosis and management service is essential for individuals who are experiencing symptoms suggestive of an autoimmune disease. While there are some limitations and potential drawbacks, the benefits of early and accurate diagnosis and effective treatment far outweigh the risks. We recommend that individuals who are concerned about the possibility of having an autoimmune disease seek evaluation from a qualified healthcare provider.
### VI. Insightful Q&A Section
Here are 10 insightful questions related to ICD-10 positive ANA, addressing genuine user pain points:
1. **Q: My ANA is positive, but my doctor says I don’t have an autoimmune disease. Why?**
* **A:** A positive ANA result doesn’t automatically mean you have an autoimmune disease. Up to 15% of healthy individuals can have a positive ANA. Your doctor is likely considering your symptoms, physical examination findings, and other test results to determine if your positive ANA is clinically significant.
2. **Q: What does the ANA titer (e.g., 1:80, 1:160) actually mean?**
* **A:** The ANA titer is a measure of the amount of antinuclear antibodies in your blood. A higher titer generally suggests a greater concentration of antibodies. While higher titers are often associated with autoimmune diseases, they can also be found in healthy individuals. The significance of the titer must be interpreted in the context of your overall clinical picture.
3. **Q: Does the ANA pattern (e.g., speckled, homogeneous) tell me which autoimmune disease I have?**
* **A:** The ANA pattern can provide clues about the potential type of autoimmune disease, but it is not definitive. Certain patterns are more commonly associated with specific diseases. For example, a speckled pattern may be associated with mixed connective tissue disease, while a homogeneous pattern may be associated with systemic lupus erythematosus. However, there is significant overlap between patterns and diseases, so further testing is needed to confirm a diagnosis.
4. **Q: What other blood tests are typically done after a positive ANA?**
* **A:** The specific blood tests ordered after a positive ANA depend on your symptoms and the suspected autoimmune disease. Common tests include: anti-dsDNA, anti-Sm, anti-Ro/SSA, anti-La/SSB, anti-RNP, anti-centromere, anti-Scl-70, and anti-Jo-1. These tests detect specific autoantibodies associated with different autoimmune diseases.
5. **Q: Can a positive ANA result be caused by something other than an autoimmune disease?**
* **A:** Yes, a positive ANA result can be caused by various factors, including infections, certain medications, cancer, and even normal aging. It’s important to discuss all your medical history and medications with your doctor to help determine the cause of your positive ANA.
6. **Q: I’ve been diagnosed with an autoimmune disease after a positive ANA. What are my treatment options?**
* **A:** Treatment options for autoimmune diseases vary depending on the specific disease and the severity of your symptoms. Common treatments include: medications to suppress the immune system (e.g., corticosteroids, methotrexate, biologics), medications to reduce inflammation (e.g., NSAIDs), and medications to manage specific symptoms. Lifestyle modifications, such as diet and exercise, can also play a role in managing your condition.
7. **Q: How often should I be retested for ANA after a positive result?**
* **A:** The frequency of ANA retesting depends on your clinical situation. If you have no symptoms and no other evidence of an autoimmune disease, your doctor may not recommend retesting. If you have symptoms or other concerning findings, your doctor may recommend periodic retesting to monitor disease activity.
8. **Q: Can my ANA result change from positive to negative?**
* **A:** In some cases, an ANA result can change from positive to negative, particularly if the initial titer was low. However, if you have been diagnosed with an autoimmune disease, your ANA result is more likely to remain positive over time.
9. **Q: What are the long-term implications of living with a positive ANA?**
* **A:** The long-term implications of living with a positive ANA depend on whether or not you have an underlying autoimmune disease. If you have an autoimmune disease, the long-term implications depend on the specific disease and how well it is managed. If you have a positive ANA but no autoimmune disease, you may not experience any long-term health problems. However, it’s important to be aware of the potential symptoms of autoimmune diseases and to seek medical attention if you develop any concerning symptoms.
10. **Q: Where can I find reliable information and support for living with a positive ANA or an autoimmune disease?**
* **A:** There are many reputable organizations that provide information and support for individuals living with a positive ANA or an autoimmune disease, including the Autoimmune Association, the Lupus Foundation of America, and the Sjogren’s Foundation. Your healthcare provider can also provide you with valuable resources and support.
### VII. Conclusion & Strategic Call to Action
Understanding the complexities of “ICD-10 positive ANA” is crucial for navigating the diagnostic process and managing your health effectively. A positive ANA result, while potentially concerning, does not automatically equate to an autoimmune disease. It’s a piece of the puzzle that healthcare professionals use in conjunction with your symptoms, medical history, and other test results to arrive at an accurate diagnosis.
Remember, early diagnosis and appropriate management of autoimmune diseases can significantly improve your quality of life and prevent long-term complications. By actively participating in your healthcare journey, asking informed questions, and seeking support from reliable resources, you can empower yourself to live a healthier and more fulfilling life. Based on expert consensus, proactive engagement with your healthcare team is the most effective way to manage a positive ANA result.
We encourage you to share your experiences with ANA testing and autoimmune disease diagnosis in the comments below. Your insights can help others who are navigating similar challenges. For more in-depth information and resources, explore our advanced guide to autoimmune disease management. Contact our experts for a personalized consultation to discuss your specific situation and develop a tailored plan.
